- Research
The family of human coronaviruses and other respiratory viruses may be capable of infecting the central nervous system. The coronavirus that causes COVID-19 also seems capable of reaching the brain. Loss of sense of smell has been reported in a significant portion of infected people.
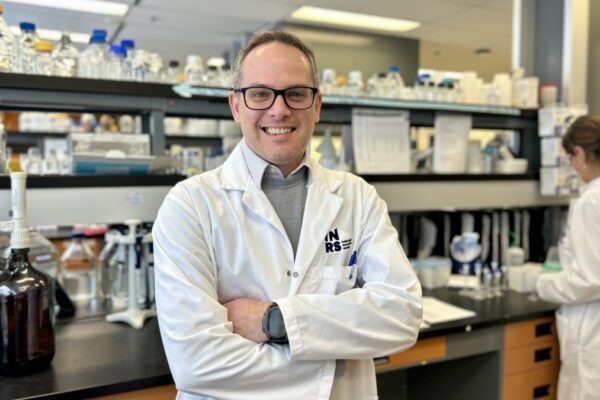
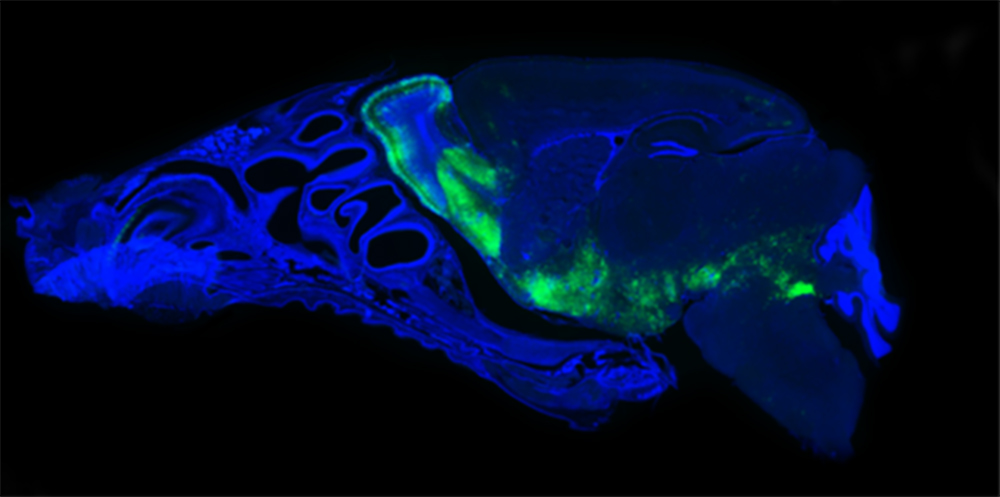
According to Professor Pierre Talbot at Institut National de la Recherche Scientifique (INRS), this could be due to an infection of the olfactory neurons. Professor Talbot’s team has highlighted similar processes in cases involving common cold coronaviruses, as described in a literature review published in the January 2020 issue of the journal Viruses shortly before the first cases of COVID-19 were reported. “Our research on the neuroinvasive and neuropathogenic capacities of human coronaviruses suggests that they can reach the smell centre of the brain, primarily via the olfactory nerve,” says the researcher, who has been studying coronaviruses for nearly 40 years.
“The first neurons infected are the neurons that detect odours in the nasal cavity,” says Marc Desforges, who worked with Pierre Talbot as a research associate for some 20 years and is now a medical biology specialist in the virology lab at Sainte-Justine hospital in Montréal. Desforges stresses that the loss of smell seems to be temporary.” Unlike most neurons in the brain, olfactory neurons can regenerate. We can therefore assume that the sense of smell will be restored once new neurons are in place.”
From the odour-sensitive neurons in the nasal cavity, the infection could potentially spread to the neurons in the smell centre via direct communication. Desforges cautions that even if the COVID-19 virus does reach the smell centre, this does not mean it will infect the rest of the brain. “The brain is well protected against viral infections by barriers. Neurons can also signal when a virus is present to summon other brain and immune cells to help fight the infection,” he adds.

Low Risk of Brain Infection
In people with weakened immune systems such as the elderly, very young children, and transplant recipients taking anti-rejection drugs, the risk of the virus effectively reaching the brain is higher than in the general population. This could potentially cause the brain to swell (encephalitis) and result in serious damage. Despite the risk, the overall likelihood of this happening remains low. “In preparing our literature review, we noted that viral encephalitis is rare. With the herpes virus, for example, the incidence of encephalitis is less than 1 in 10,000 cases,” Desforges notes. “But it’s still important to consider the risk because it’s very dangerous when inflammation does occur; the death rate is between one in two and one in four, depending on the study.”
It is too early to say whether people who recover from COVID-19 will have neurological damage, but Professor Talbot says it is a possibility. “In mice, we’ve shown that the coronavirus responsible for the common cold can cause neurodegenerative diseases with similarities to multiple sclerosis, Alzheimer’s disease, and Parkinson’s disease.” During the SARS (severe acute respiratory syndrome) epidemic in 2003, the SARS coronavirus was also found to attack the brain in a similar fashion,” he recalls. The scientific community continues to accumulate data showing that coronaviruses may be more harmful to the brain than previously thought.
About the study
Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System?, by Marc Desforges, Alain Le Coupanec, Philippe Dubeau, Andréanne Bourgouin, Louise Lajoie, Mathieu Dubé and Pierre J. Talbot, was published in thejournal Viruses. This research was supported by funding from the Natural Sciences and Engineering Research Council of Canada (NSERC) and the Institute of Infection and Immunity (III) of the Canadian Institutes of Health Research (CIHR). DOI: 10.3390/v12010014