- Research
- Science and Society
Professor Géraldine Delbès is part of an international group of scientists warning of the lack of knowledge surrounding male fertility.

Photo : Adobe Stock
Infertility now affects one in six couples of reproductive age according to the World Health Organisation. About half the time, it originates from men. As male infertility is increasing worldwide, 26 international experts including three Canadians researchers highlights that men have a right to meaningful diagnoses and targeted treatments. Unfortunately, these are currently unavailable in most cases.
The lack of knowledge regarding the causes of male infertility and in combination with limited clinical tools, has resulted in female focussed treatment—burdensome and risky invasive procedures—for male infertility.
In a consensus report published in the journal Nature Reviews Urology, the consortium of scientists led by the University of Melbourne, reveal 10 recommendations that could improve the health of men and their children, and decrease the burden on their female partners.
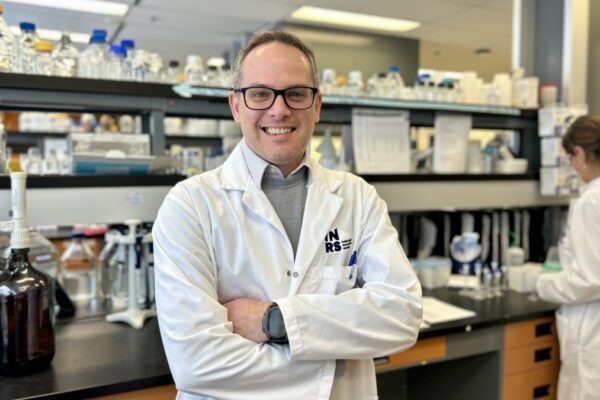
Professor Géraldine Delbès, a researcher in reproductive toxicology at the Institut national de la recherche scientifique (INRS), contributed to the report as co-author, alongside the first author, Professor Sarah Kimmins at the CHUM Research Centre (CRCHUM), and Dr. Jacquetta Trasler at the Research Institute of the McGill University Health Centre (RI-MUHC), also a co-author.
In her lab at the INRS Armand-Frappier Santé Biotechnologie Research Centre in Laval, Professor Delbès has been investigating the toxicity of environmental and medical substances on the development of male germ cells for several years.

“Several parameters linked to men’s reproductive health converge and indicate a progressive decline in fertility. However, the clinic is poorly equipped to properly diagnose and treat male reproduction. Current methods are based on outdated techniques.”
Géraldine Delbès, INRS professor researcher who specializes in reproductive toxicology
Lifestyle and environment play a key role
“The rapid decline in male fertility cannot be explained by genetics, and studies indicate that environmental factors are a driving force, says Sarah Kimmins. These include increased exposure to hormone-disrupting chemicals that exist in our daily lives and persist in the environment.”
One of the key recommendations of the report is to increase public awareness through public health campaigns around these lifestyle choices that are hazards to men’s fertility.
“As it takes months to make sperm, men should consider adopting a healthy lifestyle well before planning their families,” says Dr. Jacquetta Trasler.
Urgent Need for Better Diagnoses and Treatment
Men are currently designated infertile based on family history, physical examination, hormone profiles and a simple semen analysis that has not changed for more than 50 years.
“In fact, few biomarkers are available and those that are used are based on ancient knowledge of reproduction”, explains Professor Delbès.
According to the researcher, there has not been much progress in the clinic and this area of research is unfortunately underfunded.
“In medically assisted procreation, the way to overcome male gamete failures is largely based on treatments for the woman. It’s time for that to change! We need more resources to respond to this alarm signal, we also need to better inform and prevent, especially young people.”
Géraldine Delbès
About the 10 recommendations
1. Governments, healthcare systems, insurance companies, and the public should understand and acknowledge that male infertility is a common, serious medical condition and patients have a right to meaningful diagnoses and targeted treatments;
2. Establish a global network of registries and biobanks containing standardized clinical and lifestyle information, and tissue from fertile and infertile men, their partners, and children. Link it to national healthcare data systems;
3. Implement protocols and incentives to standardize collection of de-identified tissue and clinical/lifestyle data;
4. Fund more international, collaborative research to understand the interactions and impacts of genetic, lifestyle, and environmental factors on male fertility in diverse populations;
5. Integrate genomic sequencing into diagnosis of male infertility;
6. Develop additional diagnostic tests to improve diagnosis and cause of male infertility.
7. Rigorously test the impact on male fertility of compounds—especially endocrine-disrupting chemicals—in products, the workplace, and the environment. Implement regulations and policies and develop safe alternatives;
8. Rigorously test strategies for medically assisted reproduction before they are integrated into clinical practice;
9. Public education campaigns to promote discussion of male infertility and engagement in health seeking;
10. Improved training for healthcare workers to promote male reproductive health across the lifespan.
About the study
“Frequency, morbidity and equity—the case for increased research on male fertility,” by Sarah Kimmins et al., was published online Oct. 12, 2023, in Nature Reviews Urology.
The paper’s 26 authors are world leaders in andrology, gynaecology, urology, cellular biology, endocrinology, environmental hazards, pathology, reproductive medicine, medically assisted reproduction, oncology, genetics, paediatrics, pharmacology, and therapeutics.